Resumen
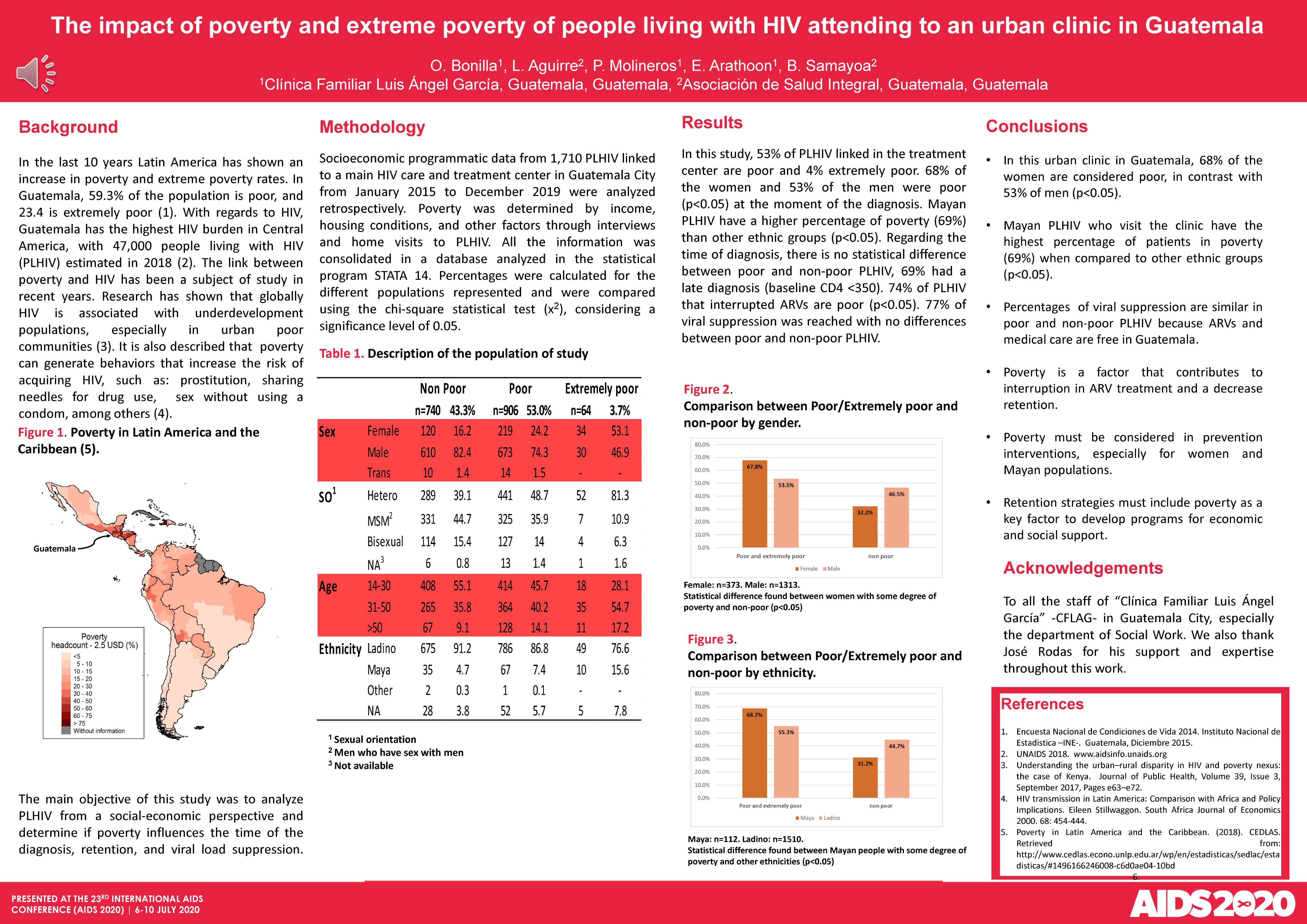
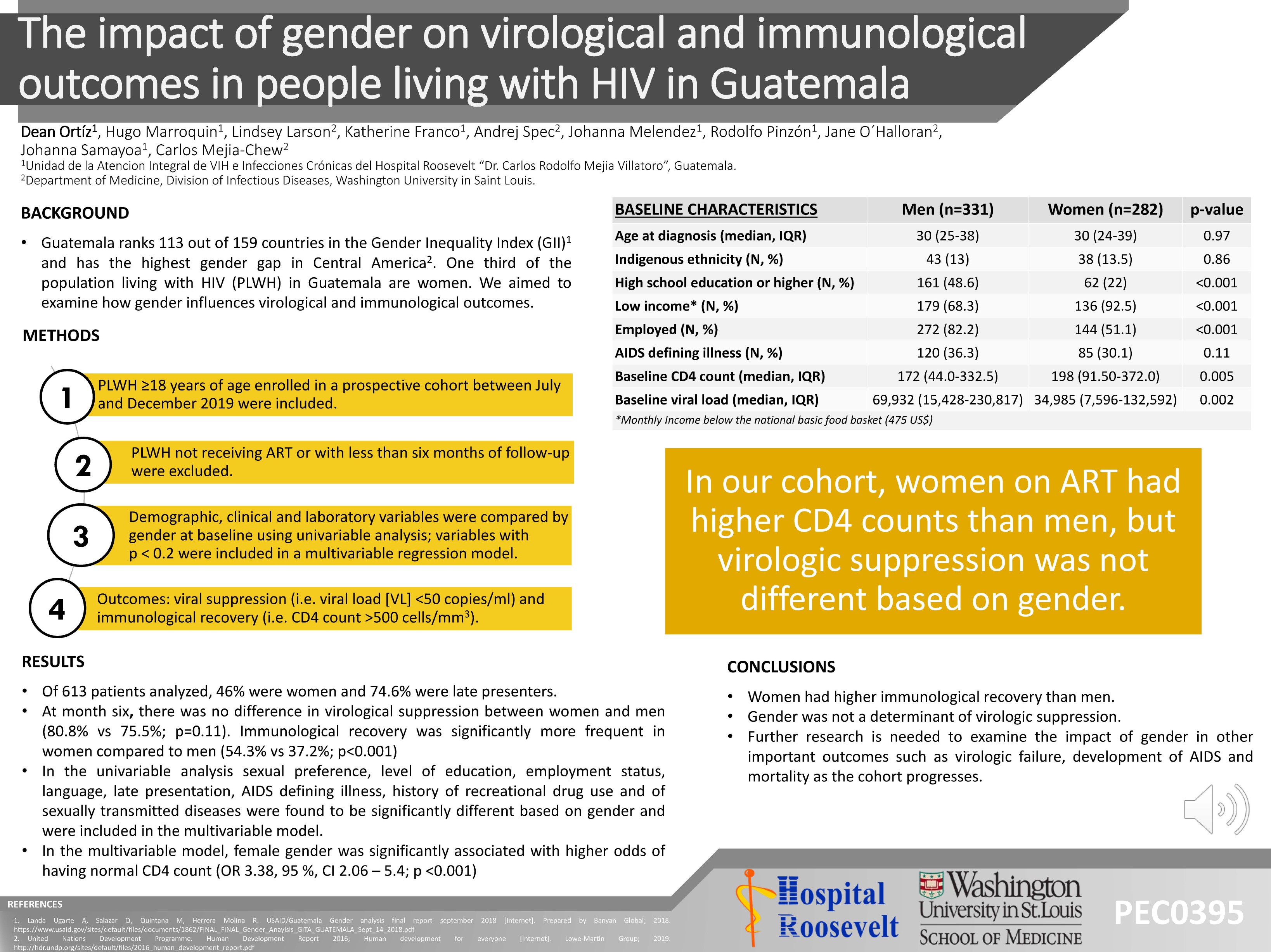
BACKGROUND: In Guatemala, 59.3% of the population is poor, and 23.4 is extremely poor. Guatemala has the highest HIV burden in Central America, with 47,000 PLHIV estimated in 2018. Poverty can generate risk behaviors to acquire HIV infection. The main objective of this study was to analyze PLHIV from a social-economic point of view and determine if being poor influences the time of the diagnosis, retention, and viral load suppression. METHODS: Socioeconomic programmatic data from 1710 PLHIV linked to a main HIV care and treatment center in Guatemala City from Jan. 2015 to Dec 2019 were analyzed retrospectively. Poverty was determined by income, housing conditions, and other factors through interviews and home visits of the PLHIV. RESULTS: 57% of the PLHIV linked in the treatment center are poor and 4% extremely poor. 68% of the women and 53% of the men were poor (p<0.05) at the moment of the diagnosis, also Mayan PLHIV have a higher percentage of poverty (69%) than other ethnic groups (p<0.05). Regarding the time of diagnosis, there is no statistical difference between poor and non-poor PLHIV, 69% had a late diagnosis (baseline CD4 <350). 74% of PLHIV that interrupted ARVs are poor (p<0.05). 77% of viral suppression was reached with no differences between poor and non-poor PLHIV. CONCLUSIONS: Poverty must be considered in prevention interventions, especially for women and the Mayan population. Retention strategies have to include poverty as a key factor to elaborate programs for economic and social support. Fortunately, percentages of viral suppression are similar in poor and non-poor PLHIV because ARVs and medical care are free in Guatemala.