Resumen
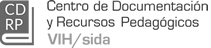
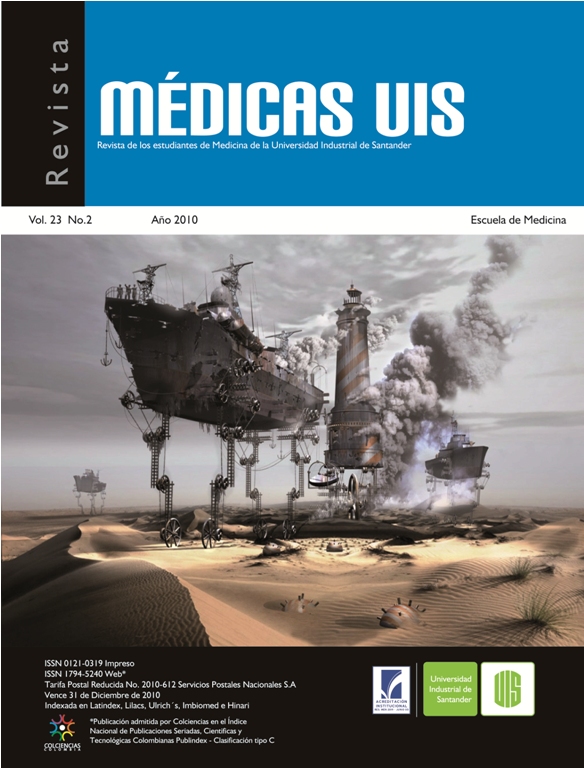
Background: Among the HIV preventing measures in most-at-risk populations, PrEP has demonstrated to be effective in reducing the risk of contracting HIV among Men who have sex with men and Transgender populations. In the Dominican Republic no previous PrEP implementation has been documented. The main objective of this pilot is to demonstrate feasibility, adherence, and effectiveness of PrEP in a cohort of MSM and Transwomen in the Dominican Republic. Methods: Self identified as MSM and Transwomen attending an outpatient clinic in the capital city were invited to receive PrEP during a period of nine months. All participants were screened for substantial risk of HIV infection by the psychology department and those qualifying were screened for HIV and other STIs including HPV by anal smear. Those with a recent sexual contact without condom were deferred for a 30 days visit or PEP. All participants were counselled about condom use with PrEP, and vaccination against Hepatitis A and B. Results: A total of 360 MSM and Trans attended the clinic during the screening period. Of those, 50% (n=180) were invited to initiate PrEP, and 90% (n=162) received PrEP. Mean adherence to PrEP was 93.1% to 30 days after initiation, and 93.1% after 120 days of initiation. Reactivity to VDRL at the baseline was 30.5% among 30-34 years old (Table 1), and among those without previous syphilis infection after 120 days on PrEP was only 2%. Conclusions: PrEP implementation in the DR demonstrated to be well tolerated and adherence was very high. Rates of syphilis infection between MSM and Trans are substantially high, however the rate of new infections after PrEP use was very low (2%). The integrated approach of PrEP implementation seems to be key for scaling-up PrEP use among other populations. Psychological support and behavioural interventions are necessary to reinforce the HIV prevention toolbox before, during, and after PrEP.