Resum
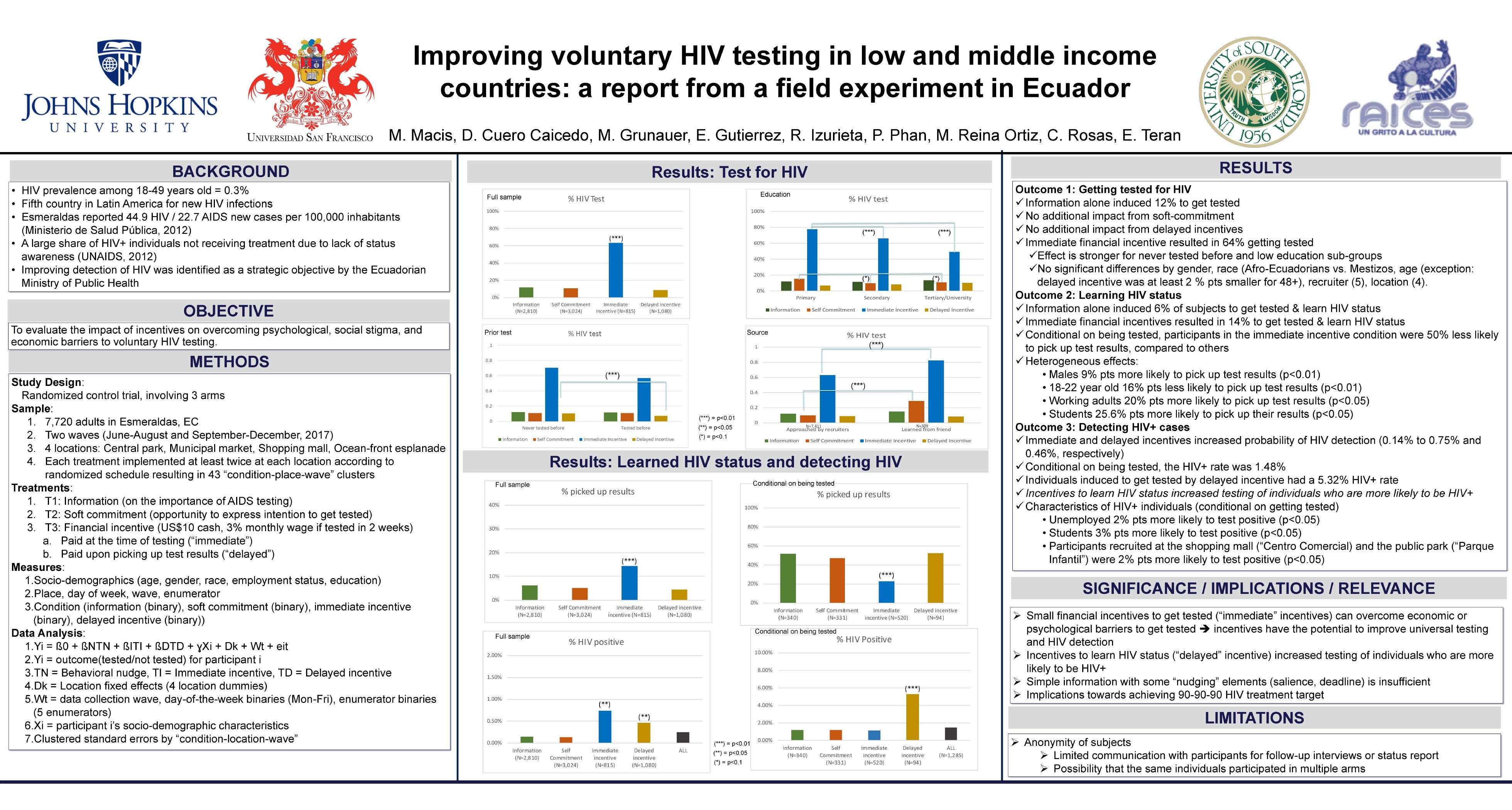
Background: HIV/AIDS prevention and control relies heavily upon timely diagnosis and treatment. UNAIDS has set the 90-90-90 target by 2020 (i.e. 90% of PLHIV know their status, 90% of those diagnosed will be under treatment, and 90% under treatment will achieve viral suppression). HIV/AIDS under-detection may stretch scarce public health resources in LMIC. We conducted a field experiment in a LMIC to test the hypothesis that a financial incentive intervention, compared to an information-only or to a behavioral nudge, will significantly increase voluntary HIV testing.
Methods: A randomized controlled trial was conducted in a large Ecuadorian city that carries a disproportionate burden of HIV/AIDS from June to December 2017. Consented participants were randomly assigned to one of three arms: 1) control arm where participants received information on HIV testing; 2) soft-commitment (behavioral nudge) arm, where participants received a narrative to overcome social stigma and activate the sense of social responsibility; and, 3) financial incentive arm where participants were offered a US$10 reward received either at time of testing or when they picked up their test results. Participants were recruited from three heavily trafficked public sites around the city. Socio-demographic information was captured using a self-administered survey. The identities of the participants were masked. Outcomes included testing rate and HIV seropositivity rate. Chi-square tests were used to compare rates across treatment arms.
Results: 7,721 participants were approached and 1,321 got tested. Randomization was effective and no systematic biases were identified. Socio-demographic variables (age, ethnicity, education and previously tested for HIV) did not differ between treatment arms (p>0.05). Testing rate was 12.2%, 11.3% and 33.5% for control, behavioral nudge and financial incentive treatment arms, respectively (p< 0.05). HIV seropositivity rate was 1.2% for participants in both control and behavioral nudge arm and 1.5% for financially incentivized participants (p>0.05). These were individuals that would have gone undetected but for the intervention.
Conclusions: Our preliminary results indicate that financial incentives provided at the time of outreach can overcome the psychosocial barriers of voluntary HIV/AIDS testing. The subsequent detection of new HIV/AIDS cases support infection control with early intervention, limit economic costs, and improve surveillance accuracy.